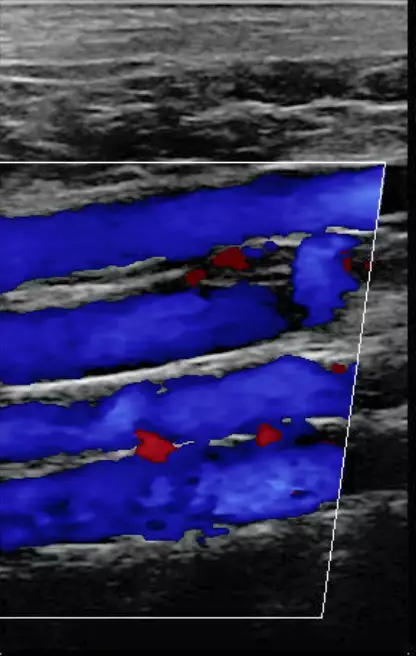
Blood clots are your body’s first line of defense against bleeding. As a response to a wound, clotting is an essential — perhaps even life-saving — function. But when the body’s normal mechanisms are disrupted, blood clots can form when they aren’t needed in places that make them dangerous. A blood clot that develops in a major deep vein is called deep vein thrombosis (DVT). DVT can pose a serious threat to your health if it is not diagnosed and treated in a timely manner.
Deep vein thrombosis is a condition in which the blood clots or forms a thrombus in one of the deep veins in your body. This occurs primarily in the lower extremities, but deep vein blood clots can also develop in other areas of the body. DVT is a serious condition because a blood clot that has formed in your vein can break loose, travel through your bloodstream and lodge in your lungs, blocking blood flow. Even if a blood clot remains in place, it may permanently damage the valves inside the vein. This damage can lead to chronic problems in the leg such as swelling, pain and leg sores.
Every year, approximately 2 million people will develop deep vein thrombosis and around 200,000 of them die. DVT kills more people than AIDS, breast cancer and motor vehicle accidents combined. It’s important to find and treat DVT early for the best prognosis.
What Causes DVT?
In the event of an injury, bleeding triggers a biological “domino effect” that sets a series of steps in motion. Platelets and proteins called coagulation factors clump together to seal the damaged blood vessel and stop the bleed. The blood clot dissolves when it is no longer needed. Blood clotting disorders can occur if the lining of a vein is damaged, if blood flow is too slow or if a condition or medication makes the blood clot more easily. DVT is the result of a clot that forms inside a deep vein and prevents blood from circulating normally through your body.
What Can Happen If DVT Is Not Treated?
Untreated DVT can lead to illness, disability, and in some cases, death. The most serious complication of DVT is pulmonary embolism — a blockage that occurs when part of the clot breaks free and travels through the bloodstream to the lungs. A small enough clot can be treatable, but a large clot can stop blood from reaching the lungs, making the condition fatal.
DVT can also damage the vein and lead to long-term complications from chronic venous insufficiency or post-thrombotic syndrome. These conditions are characterized by chronic swelling, pain, discoloration of the skin, scaling and venous stasis ulcers. The symptoms may eventually become so severe that they cause disability. But there are treatments available.